Intensive Outpatient Programs: A Comprehensive Guide
Intensive Outpatient Programs (IOPs) have become a crucial component in the continuum of care for individuals recovering from substance use and mental health disorders. These programs offer a structured yet flexible approach to treatment, allowing participants to receive high-quality care without the need for residential or inpatient services. IOPs are especially beneficial for individuals who require more support than standard outpatient treatment can provide, but who do not need the 24-hour supervision of an inpatient facility. With a focus on therapy, education, and community support, IOPs empower individuals to maintain their daily responsibilities while making meaningful progress in their recovery.
What Are Intensive Outpatient Programs (IOPs)?
Intensive Outpatient Programs are non-residential treatment options that provide comprehensive behavioral health services. Typically, IOPs require participants to attend treatment sessions multiple days a week, usually for three to five days, with sessions lasting anywhere from three to four hours per day. This structure ensures that individuals receive intensive care while maintaining the flexibility to live at home, continue working, or attend school.
IOPs often serve as a step-down level of care for individuals transitioning out of inpatient treatment or partial hospitalization programs (PHPs), though they can also serve as an entry point for those whose needs exceed the scope of standard outpatient therapy. The core components of an IOP usually include individual counseling, group therapy, psychoeducation, and relapse prevention planning. Additional services may include family therapy, case management, and medication management when necessary.
Key Benefits and Target Population
One of the primary advantages of an IOP is its adaptability to the individual's life. People struggling with addiction, depression, anxiety, bipolar disorder, or trauma-related conditions can benefit from the support and accountability that an IOP provides—without uprooting their lives. IOPs are particularly well-suited for individuals who have strong support systems at home, are medically stable, and are motivated to engage in treatment.
Participants often include working professionals, parents, students, and others who cannot commit to inpatient stays but need more structure than a weekly therapy session can offer. Many IOPs also cater to specialized populations, such as adolescents, veterans, LGBTQ+ individuals, and those with co-occurring disorders. The ability to maintain employment or family responsibilities while receiving intensive care helps improve engagement and long-term outcomes for many clients.
Core Components and Structure of an IOP
IOPs typically follow a standardized curriculum that addresses a wide range of emotional, psychological, and behavioral issues. Group therapy is often the foundation, promoting peer support and providing a safe space to process emotions and develop coping skills. Group topics may include stress management, emotional regulation, communication skills, relapse prevention, and goal setting. These sessions are usually facilitated by licensed therapists who guide discussions and offer evidence-based strategies.
Individual therapy allows clients to explore personal issues in a one-on-one setting and develop personalized treatment plans. Family therapy is also a critical aspect of many IOPs, as addiction and mental health challenges often affect the entire family unit. Educating and involving family members can strengthen recovery outcomes.
Many IOPs incorporate evidence-based practices such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Motivational Interviewing (MI), and trauma-informed care. Programs may also integrate holistic approaches like mindfulness, yoga, or art therapy to support overall wellness. Regular progress evaluations help tailor the program to the individual’s evolving needs and ensure continued effectiveness.
Effectiveness and Transition Planning
Research supports the efficacy of Intensive Outpatient Programs in treating both substance use disorders and mental health conditions. Numerous studies have shown that IOPs are as effective as inpatient treatment for many individuals, especially when the program is evidence-based and includes follow-up care. Success is often enhanced when clients have a supportive home environment, engage fully with treatment, and participate in aftercare planning.
A well-designed IOP includes discharge and transition planning from the outset. Once a participant meets their treatment goals or is ready for a lower level of care, the program typically helps them transition to standard outpatient therapy, community support groups like AA or NA, or ongoing psychiatric services. Continued care and support are critical for sustaining long-term recovery, and many programs offer alumni networks or booster sessions to reinforce progress.
FAQs - Intensive Outpatient Programs
Unlike inpatient or residential treatment—which requires patients to live on-site—I.O.P. participants return home after sessions, making this a flexible option for those with responsibilities like work or caregiving. Compared to standard outpatient programs, IOPs offer more frequent and intensive services, making them suitable for those needing significant support but not 24-hour care.
For example, someone recovering from alcohol dependence who has completed detox might enter an IOP to work on relapse prevention and coping skills while reintegrating into their daily life. Candidates should have a safe and supportive home environment and the motivation to engage in regular treatment.
Additional services may include family therapy, medication management, psychoeducation, relapse prevention, and life skills training. For example, a person struggling with depression and substance use may attend group sessions for addiction education, individual therapy to process trauma, and medication check-ins for managing symptoms.
For instance, a standard IOP might operate on a Monday-Wednesday-Friday schedule from 9 a.m. to 12 p.m. or 6 p.m. to 9 p.m., offering flexibility for participants with work or family commitments. The duration and intensity can be adjusted over time based on the individual’s progress.
For example, someone with anxiety and opioid addiction might receive medication-assisted treatment (MAT), anxiety-focused therapy, and group support that addresses triggers for both conditions. Research supports the effectiveness of dual diagnosis IOPs in improving outcomes and reducing relapse.
For example, a college student in recovery may attend an IOP in the evenings after classes, while a working parent might choose early morning sessions. This flexibility supports real-world recovery while promoting balance between treatment and daily life.
For instance, someone with a history of repeated relapses might participate in a 12-week IOP followed by step-down care like standard outpatient therapy or recovery coaching. Length of stay is usually tailored to treatment goals and ongoing evaluations.
Before enrolling, patients should contact their insurance provider or the IOP admissions team to verify benefits. For example, someone with Blue Cross Blue Shield might find that their plan covers up to 80% of IOP costs after a deductible is met.
For instance, a person completing a 30-day residential program may move into an IOP to continue working on coping strategies and relapse prevention. Alternatively, someone experiencing early signs of addiction may begin with IOP as a proactive intervention.
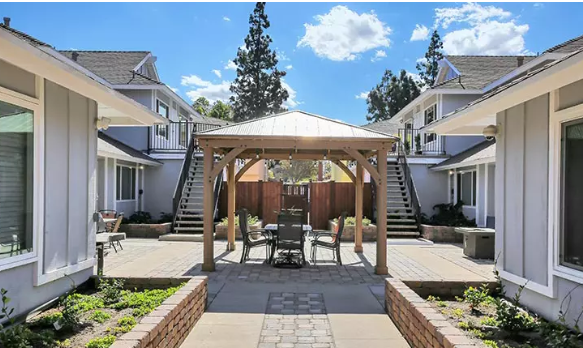
Additionally, reading reviews, touring the facility, and asking about staff qualifications, therapy models, and success rates can help you make an informed choice. For example, a local hospital’s behavioral health wing may offer an affiliated IOP with licensed therapists and psychiatrists on staff.
Summary - Intensive Outpatient Programs
Intensive Outpatient Programs provide a critical middle ground in the spectrum of behavioral health treatment, combining the rigor of structured care with the freedom of outpatient living. Ideal for individuals who need consistent, in-depth support but also have the capacity to manage daily responsibilities, IOPs are effective in addressing substance use disorders, mental health challenges, and dual diagnoses. With a focus on group and individual therapy, psychoeducation, and relapse prevention, IOPs empower individuals to recover within their communities. By offering flexibility, affordability, and clinical depth, IOPs continue to be a preferred treatment option for many people seeking to rebuild their lives in a sustainable, holistic way.
Sources
- Substance Abuse and Mental Health Services Administration (SAMHSA). “Treatment Improvement Protocols (TIP) Series.”
- American Psychological Association. “Evidence-Based Practice in Psychology.”
- National Institute on Drug Abuse (NIDA). “Principles of Drug Addiction Treatment: A Research-Based Guide.”
- Mental Health America. “Types of Mental Health Treatments.”




-svg.jpg)